This content is intended for Australians living with epilepsy.
The information in this guide is general in nature, please consult your healthcare professional for specific advice.
About this Guide
This guide has been developed with the support of people with epilepsy and healthcare experts to help you learn more about epilepsy and how to overcome challenges related to your condition. It does not replace the advice of your healthcare team, but it may provide you with a good starting point to take part in conversations about your care.
Introduction to empowerment
What are ‘patient empowerment’ and ‘shared decision-making’?
Patient empowerment
Patient empowerment is a process through which people gain greater control over decisions and actions affecting their health, though it is a concept that can be interpreted in different ways.
Patient empowerment means you have the information and tools to make smart choices about your health. It’s also about being encouraged to be part of the discussions and decisions about your treatment and care. Ultimately, it’s about recognising that you have a voice and helping you feel confident in using it.
In an ideal world everybody would feel empowered when it comes to their healthcare. Feeling empowered means having the information and support you need to take charge of your care and be truly involved in making decisions about your health. It’s about being in control of your overall well-being and making choices that can improve your happiness and make you feel better.
Shared decision-making
Shared decision-making is a collaborative approach to healthcare, where you work with your healthcare providers to make decisions about your treatment or care. Shared decision-making involves sharing information, discussing treatment options, and considering your preferences, values, and goals.
When you are involved in decisions about your care, you are encouraged to think about screening, treatment, or management options and the likely pros and cons of each. The goal is for your healthcare team to ensure that you understand your situation and all the options that are available to you, for you to share your needs and goals with them, and for you to collaboratively choose the best course of action for you. Shared decision-making respects your right to make choices about your health and helps you stay involved in your care.
You may not feel ready for shared decision-making at first. Sometimes, you need to start by feeling empowered to make those decisions.
How can I be more empowered?
Information
Having the right information is crucial for feeling empowered in your healthcare journey.
At the end of this guide you will find links to a variety of resources. You can also ask your healthcare team for more recommendations about finding trustworthy information.
Preparation
Your journey to empowerment must start with some planning. Since the time you’ll have with your healthcare team may feel a little short, and there may be long gaps between your appointments, it’s a good idea to prepare ahead of time.
It might help to keep a journal, either on paper or digital notes on your phone, so you have some notes to refer to during your consultation.
Questions
Your healthcare team will be happy for you to be actively involved in your treatment decisions and will encourage you to ask questions and request more information.
Asking questions ensures that you get the information you need and come away with knowledge that matters to you.
When developing this guide with the help of patients and healthcare providers, the latter said that the level of detail they give to patients depends on how engaged the patients seem to be in their own care. In simpler terms, the more questions you ask, the more information you will receive.
So don’t hesitate to speak up and ask questions during your appointments. It helps you stay informed and actively participate in your healthcare decisions.
You may also want to bring a family member or friend to the appointment with you for support. The first appointment in particular can be a bit overwhelming so it may help to have someone with you.

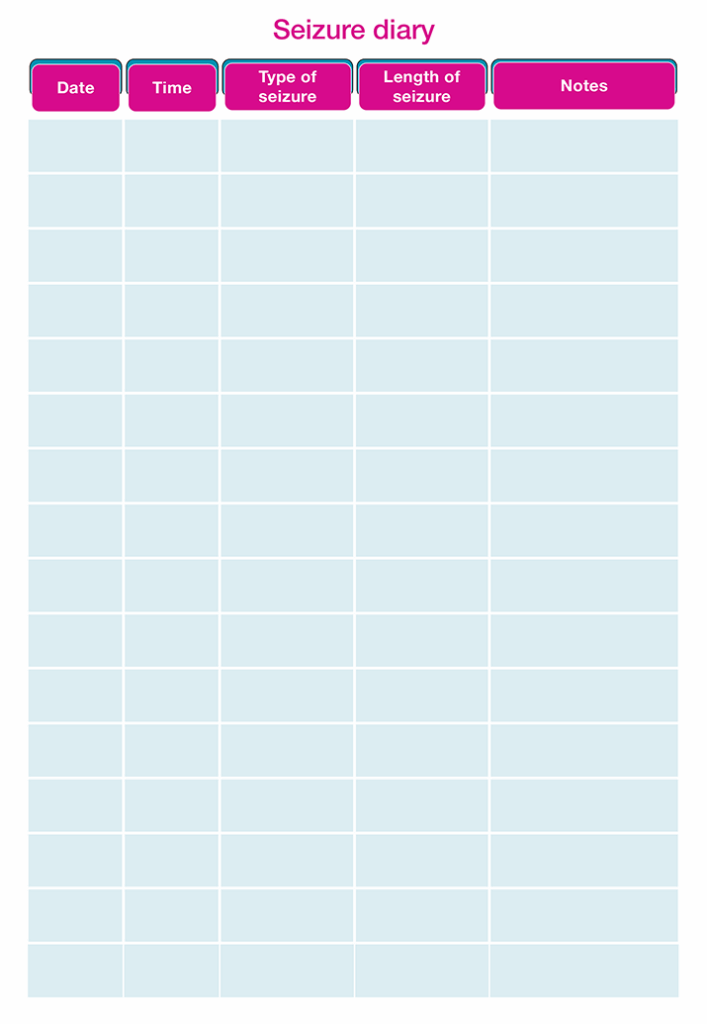
Empowerment Guide – Seizure diary
A guide to keeping track of your seizures
Knowing how often you have seizures and what happens during them are important pieces of information to gather. On top of that, tracking your seizures and keeping note of all of the details about them is a great way to become more involved in your epilepsy management. It can help your doctors to better understand your epilepsy and can be used to tailor and improve your treatment plan.
Why keeping track of seizures is a good idea
Epileptic seizures can be confusing because they come in many different forms and affect people differently. Keeping a note of the details of your seizures; what type of seizure you had, what could have triggered it, how you felt afterwards, and what would have made you feel better when coming out of your seizure can help you learn more about your own seizures and might make them feel a little less scary or daunting.
Tracking your experiences with seizures can be really helpful for your doctor or neurologist, too. It gives them a better idea of what’s happening during your seizures, how they affect you, and how they can best help you.
If you notice a change in the frequency and/or severity of seizures, talk to your doctor immediately.
Making the most of your consultation
As you manage your epilepsy, you and your healthcare team will regularly go over the goals you have set in previous appointments. Together, you’ll come up with new goals that are realistic and attainable for you. These goals are important because they will help guide your care and treatment. It’s really important to talk openly with your healthcare team about how these goals might affect your overall management of epilepsy and your treatment plan.
Here are some things you can do before, during and after your appointment:
Prepare ahead of time
Since the time you have for your appointment may feel a little short, it is essential to prepare in advance to make sure you get the most out of your interactions with your healthcare provider.
Some things to think about ahead of time are:
- New questions or concerns since your last appointment
- Hobbies, travels, or ambitions that you’d like to discuss with your doctor

Make sure you really understand what’s being said
To actively participate in discussions about your care, you need to be able to understand the information that is given to you and make sure that you are aware of all available options.
Don’t be afraid to ask your doctor to repeat what has been said if you have had trouble hearing, or to explain in a different way if you don’t understand what is being said.
Ask questions
During your appointments, it’s a great chance for you to ask questions about your care and treatment, ensuring that you understand and feel good about everything that’s going on and what will happen next. Your appointments are your opportunity to ask questions or start discussions about anything that is important to you, such as:
- Practical information regarding your treatment
- Any changes to your treatment
- Worries or concerns about symptoms or side effects
- Additional support needs for living with epilepsy

Get your goals and needs across
When discussing your treatment and care, it’s essential that your goals, preferences, and needs are taken into consideration. Below are some examples:
- I’d like to go on a night out with my friends
- I’d like to try a new sport
- I’d like to go on a long-haul flight next year
- I would like to worry about my epilepsy less
- I want to know more about starting a family

Engage in decision making with your doctor
Talk about the potential advantages and disadvantages of tests and treatments. Don’t hesitate to let your doctor know if there’s anything about your current care that you’re not happy with. Your appointments are also a good opportunity to discuss self-management and anything you can do to assist in managing your epilepsy.

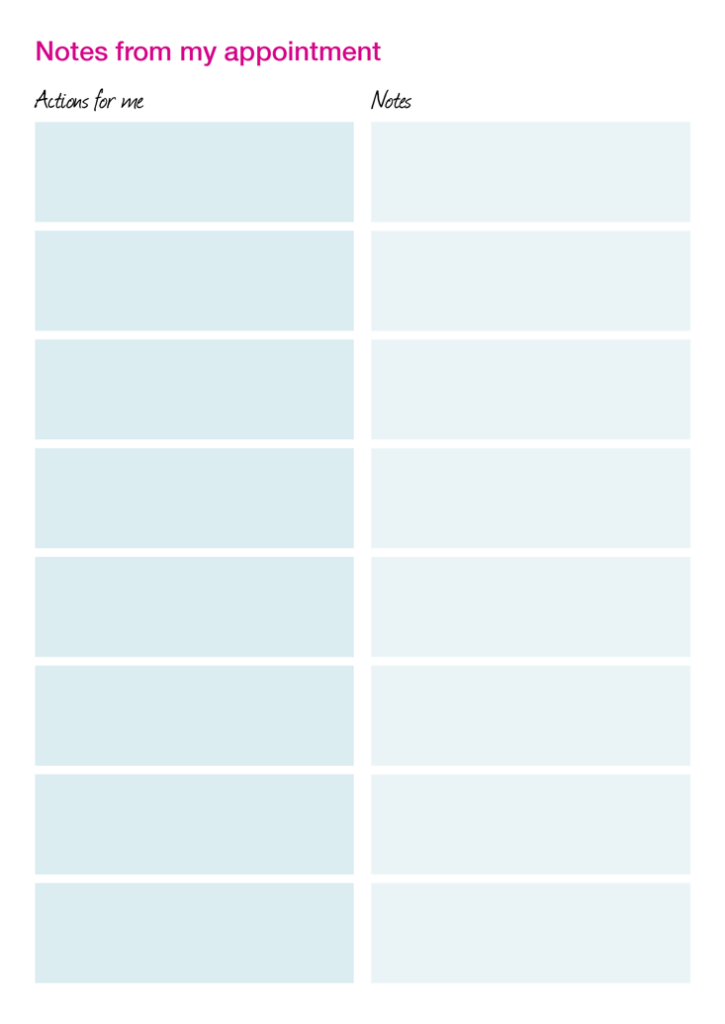
Take notes
Have you ever left an appointment and realised you can’t remember half of what you talked about? A simple way to remedy this and ensure you walk away from your appointment armed with as much information as possible is to take notes.
During each appointment, write down information on topics such as blood test results, any scheduled tests, important dates, any medications, or treatments that are discussed, and next steps. Consider keeping a dedicated folder (either physical or digital) filled with your notes and bring it with you, along with other relevant documents, to all of your appointments with your healthcare team.
Please ensure you receive medical advice for any side effects you experience. You can report side effects to the Therapeutic Goods Administration online at www.tga.gov.au/reporting-problems. By reporting side effects, you can help provide more information on safety of medicines.
Your consultation checklist
Making the most of each visit
Visits with your healthcare team can be overwhelming. A long time may have passed since your last appointment, and it can be difficult to fit in all of your questions or concerns within the allotted time for your appointment.
It’s really helpful for your healthcare team if you take a little time to gather all the information that they need beforehand. This way, it makes things easier for them and gives you more time during your appointment to talk about the things that matter to you.
This checklist has prompts for the ‘must-have’ clinical information, as well as space for you to write down your own questions or concerns in order of priority.
No question is too simple and there is no such thing as a silly question, so use the space below to highlight the topics that have been on your mind or are most the important to you in your day-to-day life with epilepsy.
Download the checklist below to record the ‘must-have’ information your healthcare team needs to monitor your epilepsy.
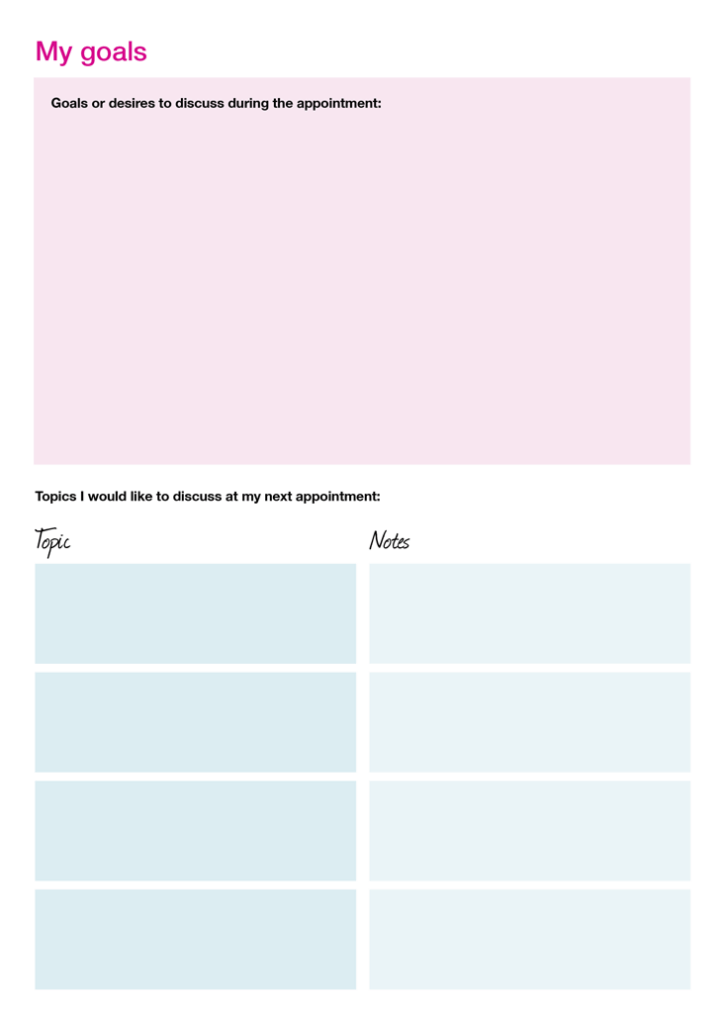
My goals
This section is where you can write down any new goals or desires you have that you would like to discuss with your healthcare team. For example, ‘I would like to take a long-haul flight in the summer. How will my epilepsy or treatment impact this?’
This section will help your healthcare team understand what topics are most important to you. Below, record any questions or concerns that you have had since your previous consultation. If the topic is very important to you and you definitely want to discuss it during your appointment, write the name of the topic in the designated space, and what you would like to discuss.
A list of example topics to discuss: mental health, sleep, work, social life, family planning, home life, finances, travel, treatment.
Quick facts about epilepsy
What you need to know
Epilepsy is a neurological disorder that affects the brain and causes recurring seizures.
Our brains are constantly filled with electrical activity, sending signals and messages between cells within the brain and from the brain to different parts of the body.
Seizures happen when a burst of intense electrical activity causes a disruption to the way the brain normally works. There are lots of different types of seizures, and what happens during a seizure depends on where in the brain the abnormal electrical activity is happening, and how far around the brain the electrical surge spreads.
During some types of seizures, the person may stay awake and aware of their surroundings, but they might experience strange sensations, feelings, or movements. In other types of seizures, they may lose consciousness and become stiff, fall to the ground, and jerk or shake.
There are lots of reasons why a person may have epilepsy, including genetic factors, brain injuries, changes to the brain, or some medical conditions.

Epilepsy is a chronic condition, which means that it is long-term and may need continuous treatment. Despite that, people with epilepsy can still enjoy hobbies, advance their career and have a fulfilling love life.
For friends and family: How to spot a seizure
There are many different types of seizures that a person with epilepsy may have, and each of them will manifest differently. Here are some common types of seizures and how to spot them:
Generalised seizures affect both sides of the brain.
- Absence seizures: these can cause the person to ‘blank out’, or stare into space. These seizures only affect the person’s awareness and do not usually cause them to fall to the ground. The person will stop all activity, stare blankly and be very still for a few moments and then continue as they were before the seizure.
- Tonic-clonic seizures: these are the type of seizure that most people recognise. During these seizures the person will lose consciousness, suddenly turn stiff, fall to the ground, and begin to convulse. They may also let out a crying sound or bite down on the inside of their mouth.

Focal seizures happen in one side of the brain.
- Focal aware seizures: can affect a small part of the brain and cause twitching or strange sensations, like tasting or smelling something strange.
- Focal impaired awareness seizures: can make someone with epilepsy feel confused or dazed. They might not be able to answer questions or follow instructions for a few minutes.
- Focal-bilateral tonic-clinic seizures: these start in one part of the brain but then spread to both sides. At first the person has a focal seizure, which then spreads to affect both sides of the brain.
Epilepsy myth-buster
Around 800,000 Australians develop epilepsy during their lifetime, yet there can still be misconceptions about the condition. Below are some common ones that should help clear them up for those who have no knowledge of it.
Myth 1: If someone is having a seizure, they will shake and jerk on the ground

Fact: Not all seizures cause symptoms like shaking and jerking. These symptoms are most commonly associated with tonic-clonic seizures but there are a range of different types of seizures which have different symptoms.
Myth 2: Flashing lights trigger seizures in everyone with epilepsy

Fact: Around 1 out of every 100 people have epilepsy, and of these people, between 3-5% have photosensitive epilepsy. Photosensitive epilepsy is when seizures are brought on by flashing lights or contrasting light and dark patterns. It is most commonly diagnosed between the ages of 7 and 19 years old; the first light-induced seizure almost always happens before age 20. Seizure triggers vary from person to person, but some common triggers can include not getting enough sleep, stress, and alcohol.
Myth 3: You should restrain a person who is having a seizure

Fact: You should never hold down or restrain a person who is having any type of seizure; doing this can cause them an injury. Instead, make sure the area around them is clear and that they have something soft to lay their head on.
Myth 4: If you have a seizure, then you have epilepsy

Fact: Seizures can be caused by many things, including alcohol withdrawal and sleep deprivation. Having one single seizure doesn’t mean that you have epilepsy. A diagnosis of epilepsy is only made after two or more unexplained seizures at least 24 hours apart from each other – even then, a neurologist may want to perform tests to find other causes.
Myth 5: When a person is having a seizure, they are in pain

Fact: When someone is having a tonic-clonic seizure, they are unconscious and do not feel any pain. Sometimes, after a long seizure, the person may have some muscle aches and their body might feel tired and weak.
Myth 6: Women with epilepsy can’t, or shouldn’t, get pregnant

Fact: Women with epilepsy can become pregnant, have healthy pregnancies, and give birth to babies who don’t have epilepsy.

Dealing with the psychological impacts of living with epilepsy
Often, the conversations that you have with your doctor, and the information you are given can centre purely around the physical challenges of living with epilepsy. However, it is important to also acknowledge the impact that living with a long-term condition like epilepsy has on your emotional and psychological well-being. For many people seizures can be unpredictable and living with such uncertainty can negatively affect your mood.
Recognising mood changes
Changes to your mood can be linked to events in your life, but they may also be related to your epilepsy treatment. It’s not always possible to be sure of the cause of mental health issues like anxiety, stress, or depression, so it’s best to speak to your doctor or pharmacist if you have any concerns.
Identifying that you feel anxious or stressed can be difficult, because you might not always experience these feelings in the same way.
Here are some common signs and symptoms to look out for:
Mind
Body

Feeling worried all the time
Tiredness

Being irritable

Struggling to concentrate

Having a hard time falling or staying asleep
Avoiding people

Your heart is beating fast or you’re having palpitations (an irregular heartbeat)

Feeling sick

Feeling shaky

Having numbness or tingling in your fingers

Sweating

Struggling to catch your breath, or breathing too fast
While the symptoms of anxiety tend to bubble gently under the surface, a panic attack is a sudden and intense episode of fear or discomfort that usually comes on without warning. Once you learn to recognise the warning signs of a panic attack you can use specific tools and strategies to stop them before they spiral out of control. However, if you think you may be experiencing panic attacks, it is important to speak to a doctor. They can help refer you to services for psychological support.

Dealing with the day-to-day impacts of epilepsy
When people think of epilepsy, the mind often jumps straight to the seizures, an all-too familiar symptom that has a huge impact on the lives of anyone affected by epilepsy. However, if you live with epilepsy, you know that that the impact can go far beyond the seizures.
Some of the challenges of living with epilepsy which may be lesser known yet are equally as important include: women’s health, navigating the workplace and driving considerations. these are elaborated on in the next section
This guide hopes to empower people living with epilepsy, and their loved ones, with the information and tools provided to help manage various day-to-day challenges.
Women’s Health
Some women may experience changes in seizure activity due to hormonal changes, particularly during puberty, ovulation and menopause.
It is important to discuss any changes in your seizure activity with your doctor, at any age or life stage.
Contraception
Some anti-seizure medications can make hormonal contraceptives (like birth control pills & implants) less effective, and as a result, less effective at preventing pregnancy.
You should discuss appropriate forms of contraception for your treatment with your doctor. They might recommend other forms of safe and effective contraception when taking anti-seizure drugs.
If you do decide that you want to have a baby, make an appointment to discuss your options with your healthcare team who will be able to give you advice regarding contraception, medication, and family planning services. Do not stop taking your anti-seizure medication without discussing it with your healthcare provider.
Pregnancy planning

Work
Having epilepsy shouldn’t prevent you from doing most jobs, but some issues may arise which can affect work or work choices. If there’s a chance you might have a seizure at work, it’s a good idea to let your employer know about that. You can draw up a seizure action plan with them that includes what happens when you have a seizure and what they can do to help you. Having an action plan at work can help you feel more at ease and in control.

Discrimination in the workplace
Having epilepsy doesn’t necessarily stop you from having a fulfilling job, however work choices can be affected by your seizures and the potential risks if seizures are uncontrolled. Even if you have good seizure control, unfortunately, some jobs are unavailable to anyone with epilepsy. For example, someone with epilepsy cannot work as a pilot, commercial truck or public transport driver.
You may find it beneficial to talk to your doctor about risk reduction or career choices. In most cases the decision to discuss your epilepsy with a new or potential employer is a personal one. If you do choose to discuss your epilepsy, the Disability Discrimination Act makes it unlawful for employers to engage in direct or indirect discrimination
Driving
If you have epilepsy, driving laws and restrictions can feel like a sensitive topic, because they can affect your personal independence and mobility. Generally, legislation allows drivers with epilepsy to drive if their condition is under control and they have not had a seizure for a specified period of time.
Since the type of epilepsy and seizure can vary between individuals, your care team will be able to provide you with advice and support on how to comply with driving rules for drivers with epilepsy.
There are also specific regulations if you need to switch, reduce, or stop your epilepsy medication. If you are switching medication, the advice you are given regarding driving will vary depending on the new medicine you are switching to. Your care team will provide you with the most up to date information that is tailored for your condition and your treatment.
There are systems in place to support people with epilepsy who need to travel. Your epilepsy care team and general practitioner will help refer you to services and programmes to help retain your ability to travel and independence.
If you have any questions about driving with epilepsy, it’s important to speak to your doctor. When someone is diagnosed with epilepsy or has a seizure, it is the legal responsibility of that person to notify the appropriate road transport authority in their state or territory.
Resources
The following links to external information sources are not developed by, affiliated with, or owned by Eisai Australia Pty Ltd. By clicking links to external resources on this page, you will be leaving our website. Any links to external resources on this website may not comply with the Australian regulatory environment. The intent of providing links to external resources is informational and is not to be considered advice. Any information provided by external resources should be discussed with your healthcare professional and does not replace their advice.
Organisations in Australia
Being a friend, family member or carer of someone with epilepsy can be difficult. Thankfully, there are many organisations across Australia working together to help support Australians living with epilepsy. Explore some of these organisations by clicking on the different states below:
UNDERSTANDING EPILEPSY
Epilepsy Action Australia
WHAT SEIZURES LOOK LIKE
Epilepsy Action Australia
LIVING WITH EPILEPSY
Epilepsy Action Australia
EPILEPSY AND YOU
Epilepsy Smart Australia
ABOUT EPILEPSY
Epilepsy Foundation Australia
MANAGING EPILEPSY
Epilepsy Foundation Australia
MYTHS AND MISCONCEPTIONS
Epilepsy Foundation Australia
DOCUMENTATION OF SEIZURES
Epilepsy Queensland
YOU AND YOUR DOCTOR (FACT SHEET)
Epilepsy Action Australia
WOMENS ISSUES
Epilepsy Action Australia
LIVING WELL WITH EPILEPSY
Epilepsy Smart Australia
EPILEPSY, DEPRESSION AND ANXIETY (FACT SHEET)
Epilepsy Action Australia
PSYCHOLOGICAL WELLBEING
Epilepsy Action Australia
- Epilepsy Action. Supporting and empowering people with epilepsy. https://www.epilepsy.org.uk/supporting-and-empowering-people-with-epilepsy- contribution-of-the-epilepsy-specialist-nurses-sense-study. Accessed March 2024.
- World Health Organization. Health Promotion Glossary. https://www.who.int/publications/i/item/WHO-HPR-HEP-98.1. Accessed March 2024.
- National Institute for Health and Care Excellence (NICE). Shared decision making. https://www.nice.org.uk/about/what-we-do/our-programmes/nice- guidance/nice-guidelines/shared-decision-making. Accessed March 2024.
- European Patients Forum. Patient Empowerment. https://www.eu-patient.eu/policy/Policy/patient-empowerment. Accessed March 2024.
- Patient Empowerment Network. What Does It Mean To Be An Empowered Patient? https://powerfulpatients.org/2018/05/22/what-does-it-mean-to- be-an-empowered-patient. Accessed March 2024.
- Epilepsy Foundation. Women and epilepsy. Available from: https://epilepsyfoundation.org.au/managing-epilepsy/women-and-epilepsy/. Accessed November 2024
- Epilepsy Foundation. Myths and Misconceptions. Available from: https://epilepsyfoundation.org.au/understanding-epilepsy/about-epilepsy/myths-and-misconceptions/. Accessed Novmeber 2024
- Epilepsy Foundation. Understanding Epilepsy. Available from: https://epilepsyfoundation.org.au/understanding-epilepsy/about-epilepsy/what-causes- epilepsy. Accessed November 2024.
- John Hopkins Medicine. Absence Seizures. Available from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/epilepsy/absence-seizures. Accessed November 2024.
- Centers for disease control and prevention. Types of Seizures. Available from: https://www.cdc.gov/epilepsy/about/types-of-seizures.html. Accessed November 2024.
- Epilepsy Foundation. General first aid for seizures. https://www.epilepsy.com/recognition/seizure-first-aid. Accessed November 2024.
- Epilepsy Foundation. Shedding Light on Photosensitivity, One of Epilepsy’s Most Complex Conditions. Available from: https://www.epilepsy.com/stories/shedding-light-photosensitivity-one-epilepsys-most-complex-conditions-0. Accessed November 2024.
- Epilepsy Action Australia. Employment. Available from: https://www.epilepsy.org.au/about-epilepsy/living-with-epilepsy/lifestyle-issues/employment/. Accessed November 2024.
AU-NEUR-25-00033 / Date of Preparation: November 2025
email: contact_australia@eisai.net
© 2025 – All copyright reserved – Eisai Australia Pty Ltd
Website created by Lateral Connections Pty Ltd